Anatomic Considerations in Rhytidectomy
David A. Sherris, M. D., and Wayne F. Larrabee, Jr., M. D.
The word rhytidectomy is derived from the Greek root rhytis ("wrinkle") and the Greek suffix ektome ("removal of an anatomic structure"). In modern times, the term rhytidectonmy is used to denote a variety of procedures involving different anatomic planes of dissection, with the common goal of eliminating wrinkles and altering the shape of the face to give a more youthful appearance. In this article, we review some of the general anatomic changes seen in the aging face, the anatomy of the various layers of the face, the anatomic structures of the face pertinent to rhytidectomy, and finally some common anatomic variations in the patient with an aging face that may influence the surgeon's choice of one procedure versus another.
THE AGING FACE
|
|
Standard structural changes of the face occur as a person ages (Fig. 1). The skull becomes thinner and smaller, with resultant increased laxity in the over- lying skin and soft-tissue envelope. Beginning at age 20 to 25, the eyebrows slowly and steadily descend from a position above the supraorbital rim downward. This ptosis of the brow, combined with excess skin of the upper eyelids (dermatochalasis) and weakening of the underlying orbital septum, results in the typical appearance of the aging eye. The weakened orbital septum and excess laxity of the skin of the lower lids allows herniation of orbital fat that results in palpebral bags.
The cartilaginous skeleton of the nasal tip weakens and broadens, resulting in tip ptosis, lengthening of the nose, and occasionally increasing airway obstruction. With progressively increasing skin laxity, resorption of subcutaneous fat, and resorption of alveolar bone, there develops a relative excess of the skin and soft-tissues envelope of the lower face and the temporal region (Fig. 2). These events lead to descent of the chin pad, loss of delineation between the jaw line and the neck, and a characteristic jowled, "turkey gobbler" neck. As aging progresses, the hyoid bone and larynx descend, making the middle and lower neck appear more prominent.' The anterior edges of the platysma muscles lose tone and separate, creating the anterior banding characteristic of the aging neck. Submental fat may prolapse between these bands, resulting in further loss of the cervicomental angle. 3 Some patients develop a relative underprojection of the malar eminences or chin secondary to redistribution of the overlying skin and soft-tissue envelope as well as the underlying fat pad. As the soft tissues of the midface descend inferiorly, laterally, and anteriorly, the melolabial fold becomes more pronounced, especially at rest. The descent of the cheek mass, as well as progressive absorption of the buccal fat pad and subcutaneous fat, results in an increased defini tion of the melolabial fold, as well as obvious hollow ing in the infraorbital region. Perioral hard tissues also resorb, especially in the edentulous patient, causing a relative excess of the skin and soft-tissue envelope.
|
|
Department of Otorhinolaryngology Head and Neck Surgery, Mayo Clinic, Rochester, Minnesota,
and Department of Otolaryngology Head and Neck Surgery, University of Washington, Seattle,
Washington
Reprint requests: Dr. Sherris, Department of Otorhinolaryngology Head and Neck Surgery, Mayo Clinic, 200 First Street Southwest, Rochester, MN 55905
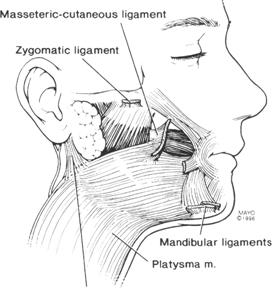
The skin varies in both thickness and adherence to underlying tissues in different regions of the head and neck. Aging results in a progressive decrease in thickness and elasticity of the skin. Heavy rhytids form, particularly at certain retaining points and at areas of repeated facial muscular activity . 5 Retaining ligaments of the face allow overlying skin to resist gravitational downward movements because they provide support from the rigid underlying bone or muscle. Furnas 6 noted four ligaments that support the soft tissues of the cheek: (1) the anterior platysmal cutaneous ligament, (2) the platysmal-auricular liga ment, (3) the zygomatic ligament (McGregor's patch), and (4) the mandibular ligaments. Recently, other authors have suggested renaming the anterior plat ysmal-cutaneous ligament the masseteric-cutaneous ligament because it originates from the anterior mas seter and actually penetrates the platysma 7 (Fig. 3).
The cheek ligaments are important in that the overlying skin and subcutaneous tissue are firmly adherent to the underlying tissues in these regions. In addition, these ligaments must be released completely during rhytidectomy procedures to assure adequate facial redraping. The platysmal-auricular ligament and the masseteric-cutaneous ligament at tach the named muscles to the dermis. The masseteric cutaneous ligament is frequently associated with multiple buccal branches of the facial nerve. The zygomatic ligament and the mandibular ligament firmly attach underlying bone to overlying dermis. The zygomatic ligament is extremely important in deep-plane and composite rhytidectomy as described by Hamra, 8 , 9 as this ligament must be released to allow full movement of the midfacial tissues. Unfortunately, release of this ligament can be dangerous, since branches of the facial nerve are commonly in close proximity.
Superficial Musculoaponeurotic System
|
|
The superficial musculoaponeurotic system (SMAS) is a continuous fibromuscular layer enveloping the face and neck that was originally described by Mitz and Peyronie. 10 As originally described, the SMAS is a fascial layer separate from and superficial to the parotid fascia. However, a significant myofascial layer superficial to and distinct from the parotid capsule is not always apparent clinically. Jost and Levet more recently suggested that the SMAS includes the layer that others have described as the parotid fascia. Anterior to the parotid gland, the SMAS has been found to be continuous with the depressor anguli oris muscle and the superficial por tion of the orbicularis oris muscle, and it includes the orbicularis oculi muscle. 5 The SMAS layer becomes markedly distinct as one approaches the mimetic facial muscles and appears grossly to merge with the fascia overlying these muscles. This is especially true as one approaches the zygomaticus major muscle in a deep-plane or composite rhytidectomy. In the anterior face, beyond the zygomaticus muscles the SMAS appears more fragile histologically. Here, it creates a mesh within the anterior face and helps coordinate the muscles of expression; however, it probably plays a smaller role in facelift surgery. 3
The upper face and associated SMAS develop from the sphincter colli profundus. 3 The SMAS in the lower face is derived from the primitive pla tysma. The frontalis muscle, the superficial temporal fascia, the orbicularis oculi muscle, the elevators of the lip, and the orbicularis oris muscle constitute the upper division. The lower division includes the true platysma and its fascia, the risorius muscle, the de-pressor anguli oris muscle, and the posterior auricular muscle. The muscles derived from the primitive platysma have limited bony insertions, in contradistinction to those derived from the sphincter colli profundus. Because the SMAS of the upper face enmeshes muscle with bony insertions, it cannot be easily moved in the facelift procedure. The junction of the two divisions of the SMAS is at the posterior border of the zygomaticus major muscle. Thus, the bony insertion of the zygomaticus major muscle tethers the SMAS at this level. In deep-plane or com posite rhytidectomy, the cutaneous facial soft tissues are completely released from this tightly inserted muscle for advancement during the procedure.
|
|
A discontinuity in the SMAS occurs at the zygomatic arch. In the temporal region, above the zygo matic arch, the SMAS, the superficial temporalis fas cia, and the temporoparietal fascia are synonymou s 3 (Fig. 4). To free the soft tissues from the zygomatic arch safely, one must stay in the subperiosteal plane, as the temporal branch of the facial nerve is other-wise at risk for injury. The temporal branch of the facial nerve above the zygomatic arch runs in the superficial temporalis fascia or the temporoparietal fascia, which is just lateral to the superficial layer of deep temporal fascia (Fig. 4). A safe way to dissect down to the zygomatic arch from above is to incise the superficial layer of deep temporal fascia approximately 2 cm above the zygomatic arch and dissect externally to the temporal fat pad that is between the superficial and deep layers of the deep temporalis fascia. More superiorly and medially, the subgaleal or subperiosteal planes of the forehead are safe for dissection in relation to the branches of the facial nerve.
Sensory and Motor Nerves
|
|
The most important sensory nerves during fore-head and facial rhytidectomy are the supraorbital, supratrochlear, and great auricular nerves (Fig. 5). The supraorbital and supratrochlear neurovascular bundles arise from their bony foramina, penetrate the SMAS, and course cephalically along the super ficial aspect of the frontalis muscle. The medial supraorbital branches penetrate the muscle more caudally, while the lateral branches run cephalically deep to the muscle for a longer distance before pene trating to the subcutaneous plane. Similarly, the auriculotemporal nerve courses with the superficial temporal vessels along the superficial temporalis fascia for a few centimeters before entering the sub-cutaneous fat layer.
The great auricular nerve is at risk for damage when the posterior flap of the rhytidectomy is elevated (Fig. 6). This nerve is especially vulnerable when the dermal attachments of the sternocleidomastoid and the platysmal-auricular ligament are dissected from the overlying skin. The most superficial part of the nerve is about 6.5 cm inferior to the bony auditory canal. This is where the nerve crosses the approximate midpoint of the sternocleidomastoid muscle. The nerve then courses superiorly and penetrates the inferior aspect of the parotid gland. The great auricular nerve is not at risk during a facelift dissection if one divides the SMAS anterior to the sternocleidomastoid 3 and dissects the skin off the muscle in the superficial subcutaneous plane. The facial nerve is the only motor nerve at risk during standard rhytidectomy procedures. The nerve exits the skull via the stylomastoid foramen and di vides within the parotid gland into multiple branches (Fig. 7). Of note, the facial nerve innervates the superficial mimetic muscles of the face on their deep surfaces. Thus, injury can be avoided if the surgeon stays superficial to these muscles during dissection. The five commonly listed facial nerve branches are the temporal, zygomatic, buccal, mandibular, and cervical. Clinically, multiple branching patterns exist that are not of any relevance during surgery. More importantly, one must understand where the facial nerve typically rests anatomically in relation to ma jor structures. The zygomatic and buccal branches of the nerve first divide in the parotid gland, and then course across the masseter muscle and buccal fat pad, lying just deep to the SMAS (Fig. 7). Multiple anastomoses are typically present between the zygo matic and buccal branches.
|
|
|
This is important during deep-plane or composite rhytidectomy procedures, as damage to one of these peripheral branches carries a good prognosis for recovery. The temporal and mandibular branches are more at risk for permanent injury, as they tend to be terminal branches. The temporal branch of the facial nerve exits the parotid and courses over the zygomatic arch and temporally within the SMAS (Fig. 4). There are usually four rami crossing the arch. The most posterior ramus is always anterior to the superficial temporal vessels, and is usually just anterior to the hairline at the level of the lateral canthus.' 3 There are two safe planes for dissection that provide access to the zygo matic arch region if necessary. One plane extends directly on the superficial layer of deep temporal fascia to the level of the zygomatic arch. The other plane is deep to the superficial layer of deep temporal fascia and deep to the periosteum across the zygomatic arch; it provides access to the bone of the zygomatic arch. One can estimate the course of the temporal branch by drawing a line from the bottom of the earlobe to a point at the lateral extent of the brow and to a point at the highest forehead rhytid. 14 The nerve, except for the auricular ramus, is situated within this triangle. The course of the marginal mandibular nerve is mostly inferior to the ramus and body of the mandible during the extraparotid course (Fig. 8). Typically, the nerve is 1 to 2 cm below the body of the mandible. The nerve remains deep to the platysma at all times, and any dissection superficial to the platysma is safe with regards to this branch of the nerve. Anterior to the facial artery, the facial nerve crosses the inferior border of the mandible and innervates the depressors of the mouth. The branches of the marginal mandibular nerve are extremely well protected until one dissects to within 2 cm of the oral commissure.
Mimetic Facial Muscles
The mimetic muscles of the face most important in rhytidectomy surgery as well as in the aging process are the corrugator supercilii, procerus, frontalis, orbicularis oculi, depressor supercilii, zygomaticus major and minor, and platysma (Fig. 9). The frontalis muscle, a major brow elevator, is routinely divided in traditional forehead rhytidectomy. In the endoscopic forehead rhytidectomy procedure, the frontalis muscle is preserved, leaving the patient with a dynamic brow in proper position. By treating the corrugator supercilii, depressor supercilii, and procerus muscles with excision or lysis, glabellar frown lines and horizontal glabellar creases can be minimized, giving a more natural result. The zygomaticus major and minor muscles are important in facelift because they provide a land- mark for the appropriate plane of dissection in deep -plane and composite rhytidectomy (Fig. 10). The orbicularis oculi muscle is important in that a portion of it is commonly excised in upper-eyelid surgery, and it is incised and resuspended in most external lower-eyelid procedures. In addition, release at the arcus marginalis is necessary in endoscopic browlift procedures, as well as composite rhytidectomy procedures, for proper repositioning of the brow and lower lid, respectively. The platysma muscle acts as a depressor of the lower lip and is innervated by the cervical branch of the facial nerve. Injury to the cervical branch of the facial nerve can result in lower-lip abnormalities similar to those seen with marginal mandibular nerve injury, but to a lesser degree. Posteriorly and superiorly, the fibers of the platysma pass posterior to the angle of the mandible. The fibers in the mid- line form an inverted V in the submental region. The peak of the inverted V is variable from the inferior border of the mandible to the level of the thyroid cartilage. Laxity and loss of tone of the platysma with aging cause platysmal banding and are more problematic in cases in which the muscle is broadly dehiscent in the midline. We routinely plicate the platysma with permanent sutures during rhytidectomy procedures. This maneuver creates a sling across the neck so that when the SMAS flap or the composite rhytidectomy flap is pulled laterally, a youthful-appearing, smooth neck results.
|
Figure 9. The mimetic muscles of the face. The super ficial muscles are cut >away on the heft for better visualization of the deep muscles. |
Vascular Supply
The primary blood supply to the face occurs via branches of the external and internal carotid arteries. Musculocutaneous penetrating branches of the facial and infraorbital arteries anteriorly supply most of the face anteriorly, and various fasciocutaneous arteries supply the face posteriorly. More importantly, the blood supply to each of the standard rhytidectomy flaps varies significantly. The standard subcutaneous and SMAS two-layered facelift effectively divides the skin from its underlying perforating branches. The subcutaneous skin flap is based solely on the subdermal plexus, which is supplied by muscular cutaneous arteries arising from branches of the facial and infraorbital arteries. A recent study by Schuster et al, 15 comparing the vascular anatomy of basic skin flaps in the subcutaneous and SMAS rhytidectomy, the composite rhytidectomy, and the subperiosteal rhytidectomy, demonstrated that the best blood supply was evident in the subperiosteal flap, where essentially no major vascular pathways were interrupted. The composite flap was found to be more vascular than the subcutaneous and SMAS flap but less vascular than the subperiosteal flap. The composite lift resulted in blood flow through a single choke zone at most. The authors found that if the subcutaneous and SMAS dissection was carried across the middle arcade of the face, then the blood flowing to and from the flap had to travel through two choke zones. The more choke zones blood has to flow through, the greater the demand on the undisturbed choke zones to provide adequate blood flow to supply the flap. In turn, the more medially the dissection is carried, the less peripheral perfusion to the flap. Yet, one must consider whether this study demonstrates significant clinical relevance, as each of these techniques has been used for many years with reasonably low flap-perfusion complication rates. Of course, the more tenuous the flap, the less likely it is to survive in suboptimal conditions (in-creased tension of wound closing, patients who smoke, patients with small-vessel disease).
OPERATIVE VARIATIONS
Hairline The position of the hairline is important in planning both forehead rhytidectomy and facial rhytidectomy. In the female patient with a high frontal hairline who requires forehead rhytidectomy, consideration should be given to a pretrichal incision and standard open approach. This will result in a stable hairline or possibly inferior descent of the hairline. In men with male pattern baldness or at risk for androgenic alopecia, and in women with a normal or low hairline, the endoscopic approach to forehead rhytidectomy is preferred. The temporal aspect of this incision can be connected to a facelift incision if the facelift is done simultaneously. Brow asymmetry secondary to unilateral facial nerve paralysis is best treated with a direct or midbrow lift. The position of the temporal hair tuft in relation to the lateral brow and the low aspect of the sideburn in women, and the level of the hairline above the ear, are also important considerations in periauricular incision placement in women (Fig. 11). When the temporal tuft is large and the distance between the lateral brow and temporal tuft is small, the sideburn is low, and the hairline above the ear is low, the rhytidectomy incision can be extended right across the hairline. If the hairline above the ear is naturally high or is high from previous rhytidectomy procedures, a V-Y flap should be incised in the skin tissue above the ear and between the superior helix and the hairline (Fig. 11B). The inferior aspect of the inci sion is then brought along the inferior border of the sideburn.
|
|
Periauricular Incision
The incision at the level of the ear can be in a preauricular crease, at the tragal edge, or on the i nside surface of tragus. In men, it is standard practice to use a preauricular rhytid so as not to bring hair-bearing skin onto the tragus (Fig. 12). In women with thicker skin, we prefer a preauricular incision, as pulling thicker skin on the tragus gives an unnatural look. In women with thin skin, a tragal edge incision is preferred because it is inconspicuous along the tragal subunit border. If one tries to make the incision on the inside surface of the tragus, the cartilage itself tends to flare out laterally and ap pears unnatural. In addition, the skin to replace that removed from the tragus and pretragal region needs to be thinned to the subdermal plexus. Sutures from the dermis to the SMAS in the pretragal region help to re-create a natural pretragal depression.
Choosing the Dissection Plane
In patients who present for facelift at a younger age, excellent results can usually be achieved with browlift and subcutaneous and SMAS facelift. Pa tients who present for an initial operation later in life typically require forehead lift, lower-lid blepharoplasty, and composite rhytidectomy. This triad of procedures treats most of their age-related concerns. The composite rhytidectomy is especially useful in older patients who present for primary facelift with deep nasolabial creases. The composite rhytidec tomy is less useful in obese patients because of poor delineation of the deep plane beyond the parotid gland.
Adjunctive procedures offered to selected patients include carbon dioxide laser skin resurfacing, and secondary upper-lid blepharoplasty 3 months or more after initial surgery. Occasionally, skeletal augmentation may also be necessary at the time of facelift. Chin augmentation or mentopexy is commonly needed. Less commonly, malar or submalar augmentation may also be necessary. We routinely plicate the platysma and perform submental and neck liposuction during the rhytidectomy procedure to prevent the formation of platysmal bands in the future and to provide a more youthful-appearing neck.
CONCLUSION
The last 10 years have been an exciting time in esthetic facial surgery. Multiple procedures utilizing different anatomic dissection planes than the more classic procedures have come into vogue. As long as the experienced surgeon is well aware of the intricacies of head and neck anatomy, these procedures can be done safely. Each new procedure carries with it a group of risks and benefits, some relevant to the anatomic plane of dissection. A thorough knowledge of anatomy as it pertains to rhytidectomy will provide confidence and adeptness to the surgeon who undertakes these new procedures.
REFERENCES
- Larrabee WF, Caro I: The aging face. Postgrad Med 74:37-46, 1984
- Gonzalez-Ulloa M, Florez ES: Senility of the face: basic study to understand its cause and effects. Plast Reconstr Surg 36: 239-246, 1965
- Larrabee WF, Makielski KH, Cupp C: Facelift anatomy. Facial Plast Surg Clin North Am 1:135-152, 1993
- Yousif NJ: Changes of the mid-face with age. Clin Plast Surg 22:213-226, 1995
- Yousif NJ, Mendelson BC: Anatomy of the midface. Clin Plast Surg 22:227-240, 1995
- Furnas DW: The retaining ligaments of the cheek. Plast Reconstr Surg 83:11-16, 1989
- Stuzin JM, Baker TJ, Gordon HO: The relationship of the superficial and deep facial fascias: relevance to rhytidectomy and aging. Plast Reconstr Surg 89:441-449, 1992
- Hamra ST: The deep plane rhytidectomy. Plast Reconstr Surg 86:53-63, 1990
- Hamra ST: Composite rhytidectomy. Plast Reconstr Surg 90: 1-22, 1992
- Mitz V, Peyronie M: The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg 58:80-88, 1976
- Jost G, Levet Y: Parotid fascia and facelifting: a critical evalu ation of the SMAS concept. Plast Reconstr Surg 74:42-51,1984
- McKinney P, Gottlieb J: Relationship of the greater auricular nerve to the SMAS. Ann Nast Surg 14:310-314, 1985
- Bernstein L, Nelson RH: Surgical anatomy of the extra-parotid distribution of the facial nerve. Arch Otolaryngol 110:177-183, 1984
- Correia PL, Zani R: Surgical anatomy of the facial nerve as related to ancillary operations in rhytidectomy. Plast Recon str Surg 52:549-552, 1973
- Schuster RH, Gamble WB, Hamra ST, Manson PN: A comparison of flap vascular anatomy in three rhytidectomy techniques. Plast Reconstr Surg 95:683-690, 1995