Testimonials
Before & After
Facial Plastic Surgery
Welcome to Our Buffalo, NY, Practice Experience World-Class Care at The Clinic of Facial Plastic Surgery
Facial plastic surgeon David Sherris offers a full range of both surgical and non-surgical facial rejuvenation procedures at his Buffalo, NY, plastic surgery office. He serves patients from nearby communities and throughout the world. Dr. Sherris’ skill and expertise as a surgeon can help you achieve natural-looking results whether you are interested in a surgical procedure like a facelift or rhinoplasty, or just want to refresh your appearance with BOTOX® Cosmetic or a filler like Restylane®.
Our plastic surgeon's artistry can not only improve the way you look but also change the way you feel about yourself. Let David Sherris, MD, and his team at The Clinic of Facial Plastic Surgery help you start your new beginning.

"They can expect me to do the best job I possibly can..."
Rhinoplasty Before and After
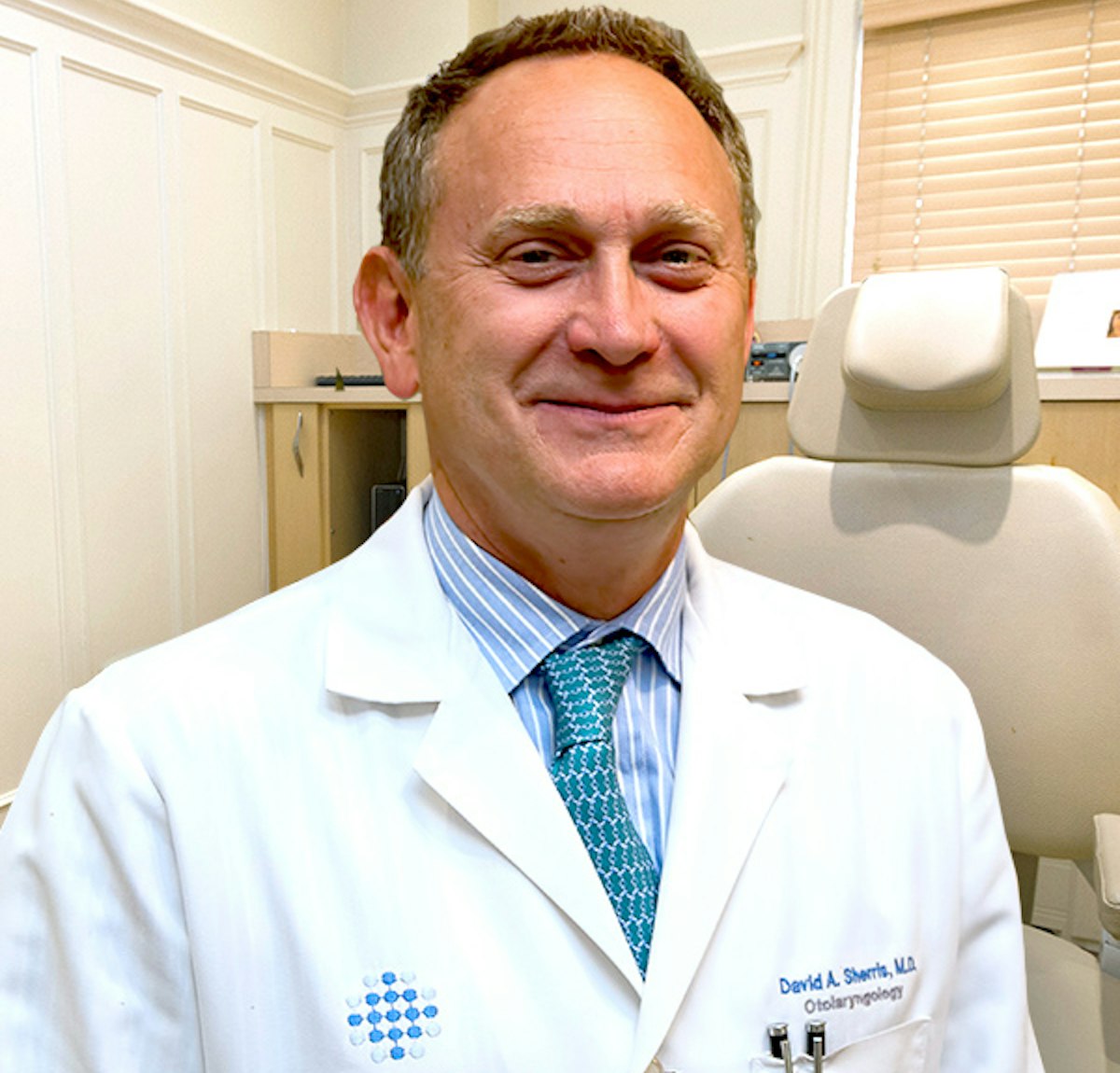
Meet the Doctor
Dr. David A. Sherris is double board-certified and fellowship-trained. He offers today’s most advanced facial plastic and reconstructive procedures.
Our surgeon is the former chairman of the Facial Plastic Surgery Division of the world-renowned Mayo Clinic. His skill, expertise, and ability to achieve beautiful and natural-looking results have helped him gain the admiration of his peers and the gratitude of thousands of patients from all over the world.
Many patients have traveled to his plastic surgery office in Buffalo, NY, including royal families, Hollywood celebrities, Fortune 500 company leaders, entertainers, politicians, and other surgeons.
David Sherris, MD, is affiliated with professional organizations including:
- American Academy of Facial Plastic and Reconstructive Surgery
- American Board of Facial Plastic and Reconstructive Surgery
- American Board of Otolaryngology

Take the First Steps Towards a New You
Facial plastic surgeon Dr. Sherris and his team of compassionate professionals at The Clinic of Facial Plastic Surgery in Buffalo, NY, can help you look younger and feel more confident in your appearance. Whether you are considering surgery or non-surgical treatment, Dr. Sherris can help you achieve the results you desire.
During a consultation at our plastic surgery clinic, D. Sherris can answer any questions you have regarding treatment so that you can make an intelligent decision towards reaching your aesthetic goals.
Call our friendly team to begin:
(716) 884-5102
"Professional and transparent." Patients Appreciate Our Buffalo Plastic Surgeon
I felt completely confident and comfortable in my decision to move forward with Dr. Sherris and his staff. They were professional and transparent through the entire process!
View on GoogleRhinoplasty done a year ago. Dr. Sherris was wonderful. Everything was explained start to finished. Everyone in his office are very nice and professional. I am happy with my results and my nose looks great and most importantly I can breathe!
View on GoogleOur Services
Non-Surgical Treatments
Featured Procedures
Rhinoplasty
If you are unhappy with the appearance of your nose, rhinoplasty can increase your confidence and balance your features. David Sherris, MD, is one of a select group of plastic surgeons who specialize in rhinoplasty.
Facelift
While there are many benefits to maturity, sagging and wrinkled skin can cause your facial features to lose definition. A facelift can help you achieve a more youthful look by smoothing wrinkles and tightening the skin.
Blepharoplasty
Bags under the eyes and sagging eyelids can make you appear constantly tired and can compromise your field of vision. Buffalo plastic surgeon Dr. Sherris can perform surgery of both the upper and lower eyelid for a rejuvenated, rested, and alert look.
Injectables
Non-surgical treatments can smooth facial creases, restore lost volume, and minimize other telltale signs of aging. We use effective, subtle injectables like BOTOX® Cosmetic, JUVÉDERM®, Restylane®, RADIESSE®, and Sculptra® Aesthetic.
The Stunning Results Of a Facelift
"Dr. Sherris gave me my quality of life back." Patients Praise David Sherris, MD
Very satisfied with the surgery dt. Sherris performed and the treatment I received from him and his staff. Very professional helpful and friendly. Dr. Sherris makes you feel very comfortable and at ease. Takes time with you and answers any questions you may have. Very impressed with dr Sherri snd his staff. Would highly recommend
View on GoogleI cannot recommend Dr. Sherris (and everyone who works in his office) enough. He made me feel incredibly comfortable throughout my procedure, and while I was healing from a traumatic injury. One of his recovery nurses also gave me her personal phone number, and was available to answer any questions I had in the days following my surgery. I feel like Dr. Sherris gave me my quality of life back, and I am so very grateful.
View on GoogleStart Planning Your Enhancement Meet With Dr. Sherris to Talk About Your Goals
Buffalo plastic surgeon Dr. Sherris has earned the trust and gratitude of many patients due to his honest approach steeped in experience and expertise. He is not a doctor who will simply create a checklist of the changes you want and book your surgery. Instead, he will provide recommendations and discuss treatments he believes will be truly beneficial to you by harmonizing with your natural features and allowing you to look like a rejuvenated version of your best self.
While Dr. Sherris' resume makes his capabilities and reputation clear, it is equally important to gain a sense of who your surgeon is as a person, and the type of bedside manner you can expect at every stage of your treatment. During your private consultation at his Buffalo, NY, office, you will have the opportunity to ask as many questions as you like, explain your goals in great detail, and consider his feedback regarding the best way to realize the changes you desire. To request your consultation, please write to us or give us a call:
Welcome to Our Office Take a Virtual Tour
Flexible Financing Available

To help patients manage out-of-pocket plastic surgery expenses, our surgical clinic offers flexible payment plans through CareCredit®. CareCredit provides financing options that range from six to 60 months. This allows you to receive the treatment you want while maintaining your monthly budget.
Frequently Asked Questions
Does insurance cover rhinoplasty?
It depends on why you are undergoing the surgery. If you have been injured or if a deviated septum is interfering with your breathing, insurance may contribute to the cost of rhinoplasty. If you are undergoing the surgery for cosmetic purposes, insurance will not cover the cost.
Does insurance cover procedures performed for reconstructive purposes?
If you have reconstructive needs, many insurance policies will contribute to the cost of your treatment. Our team will gladly contact your provider on your behalf to determine if the reconstructive surgery procedure you need is covered, and to help maximize your benefits.
What is the difference between a full facelift and a mini facelift?
While a full facelift can address the entire face, from the brow to the chin, a mini facelift focuses only on the lower third of the face.
I'm not ready for plastic surgery. Which non-surgical facial rejuvenation treatments are right for me?
The only way to know which non-surgical rejuvenation procedure can achieve your goals is to schedule a consultation with a reputable plastic surgeon.
Where does Dr. Sherris perform surgery?
Most procedures are performed in an accredited hospital. Less extensive procedures, such as blepharoplasty, can be performed in our Buffalo office using local anesthesia. During your consultation, Dr. Sherris will be able to tell you where your surgery will take place, based mainly on the extent of the procedure.
Why should I consider Dr. Sherris?
Buffalo plastic surgeon Dr. Sherris is certified by both the American Board of Facial Plastic and Reconstructive Surgery and the American Board of Otolaryngology. He focuses exclusively on facial procedures. Since 2005, he has been regularly named among the "Best Doctors in America" by his colleagues, and has been trusted by royalties, celebrities, and politicians. As the former chairman of the Facial Plastic Surgery Division of the Mayo Clinic, Dr. Sherris is considered a leader in his field. During a consultation, you can find out for yourself why he has earned the trust and admiration of so many.
"The best decision I have ever made!" More Praise for Our Buffalo Plastic Surgeon
The best decision I have ever made! So happy with my results , Dr.Sherris is the only person I’d trust with my face ! His staff is also amazing !
View on GoogleWow, I recently had an endoscopic brow lift and an upper blepharoplasty and the before and after pictures are incredible. I look so well rested and my peripheral vision has greatly improved. I highly recommend Dr. Sherris and his staff.
View on Google










